Easy Information Technology Cancer Patient Senior Projects
Computer science uses hardware, software, algorithms and data collection to shape how researchers and oncologists develop the most personalized and effective cancer treatment.
Robotic-assisted surgery, which is a technology with growing potential, is the most tangible example of computer science working to treat cancer with greater precision than traditional surgical procedures.
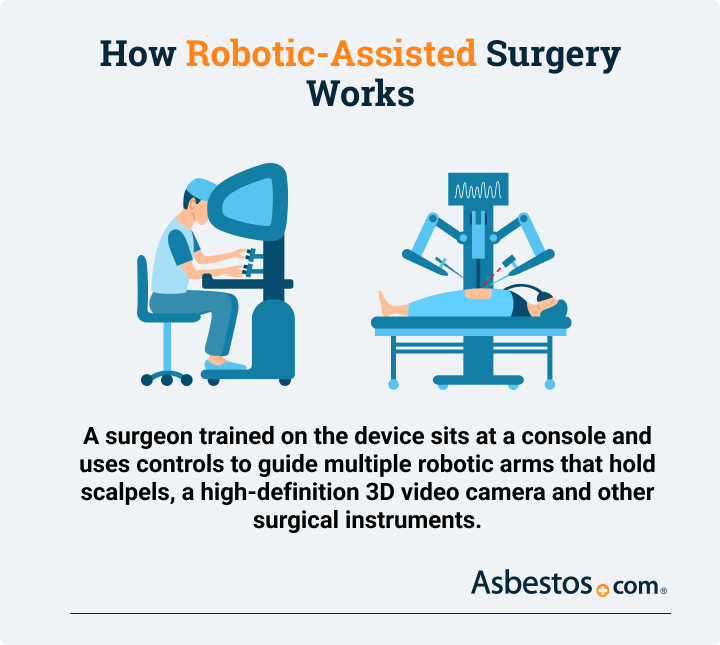
How Does Robotic-Assisted Surgery Work?
A surgeon trained on the device sits at a console and uses controls to guide multiple robotic arms that hold scalpels, a high-definition 3D video camera and other surgical instruments.
In 2021, several U.S. cancer centers, including University Hospitals in Cleveland, started using the Monarch Platform. This device is another robotic-assisted tool that obtains biopsies from hard-to-reach nodules deep in patients' lungs.
The goal of this type of robotic surgery: Earlier lung cancer diagnoses can lead to earlier treatments and improved long-term results for cancer patients.
The Monarch Platform builds upon robotic treatment technology started by the da Vinci surgical system, which was first used in cancer treatment in 2001.
Computer technology has massive potential for the future of cancer treatment, especially in the evolving fields of artificial intelligence, virtual reality, implantable sensors and other technologies.
Over 86% of prostate cancer surgeries in the United States are robot-assisted operations.
Source: Nature, 2020
Could AI Lead to Cancer Breakthrough?
Cancer researchers are making strides using artificial intelligence, also known as AI, in the early diagnosis of cancers, development of new cancer treatment and preventing cancer tumor growth.
Artificial intelligence is a computer software that relies on a series of instructions to accomplish a useful task. These instructions are called algorithms that function like directions in a pie recipe.
Researchers at Case Western Reserve University and Cleveland Clinic, among other Ohio cancer centers, ran a limited study in 2020 to see if AI could determine whether immunotherapy promoted cancer growth in a small subset of lung cancer patients.
The results showed that using AI to analyze CT scans of tissue identified biomarkers that could show which of the 109 non-small cell lung cancer patients in the study would experience tumor growth from immunotherapy.
Researchers will use that technology to teach computers to make AI better at detecting cancer and other diseases.
"In 5 to 10 years' time, I hope we will see personalised immunotherapy. This means that doctors - probably through a computerised AI algorithm - would be able to incorporate information about the individual, their tumour, their immune system, and their genetics to create a personalised prescription for the type of immunotherapy or combinations that would be most likely to work for that person."
Dr. Anna Nowak
Mesothelioma researcher at The University of Western Australia
AI could improve the medical scan image quality of MRI and CT machines. It would also reduce patients' radiation exposure by increasing the scan's precision. Researchers developed one of the earliest AI programs in 1965, named DENDRAL, and it helped chemists discover unknown forms of medications.
Another advantage: AI will be a more cost-effective alternative for drug discovery and development. AI programs can check for new uses of existing medications and reduce the burden on expensive clinical research.
Can AI cure cancer? At this point, no. But the data-sharing aspect of AI and its untapped possibilities could lead to finding a cure for cancer or other advances in cancer treatment.
Advances in Cancer Research with Virtual Reality
While virtual reality for cancer patients has not advanced to the level of a potentially curative treatment, it has shown progress in cancer symptom management.
Virtual reality, also known as VR, lets patients interact with a simulated environment through special goggles. The device replaces the user's sight with an imaginary scene.
Some simulations feature relaxing environments such as a beach with the sound of waves and birds. Others may provide educational scenes that show how a cancer patient is diagnosed.
A study published in the Journal of Cellular Physiology in 2020 showed that breast cancer patients using VR while undergoing chemotherapy showed improvements in their moods.
The patients were immersed in scenes involving animals and nature, according to the study. These women showed less anxiety, depression and fatigue than the other women who were not exposed to virtual reality during therapy.
Researchers say those types of results show VR can lead to improved psychological support for cancer patients as a palliative treatment, and that could translate to better survival and quality of life.
Moffitt Cancer Center in Tampa also partnered with Ringling College of Art and Design in 2020 to create a VR program to help reduce stress in cancer patients, connect them to survivor stories and help them better understand their cancer treatment.
Virtual reality is far from becoming a cure for cancer, but the advanced cancer technology may lower patients' stress levels, which could lead to improved cancer survival rates.
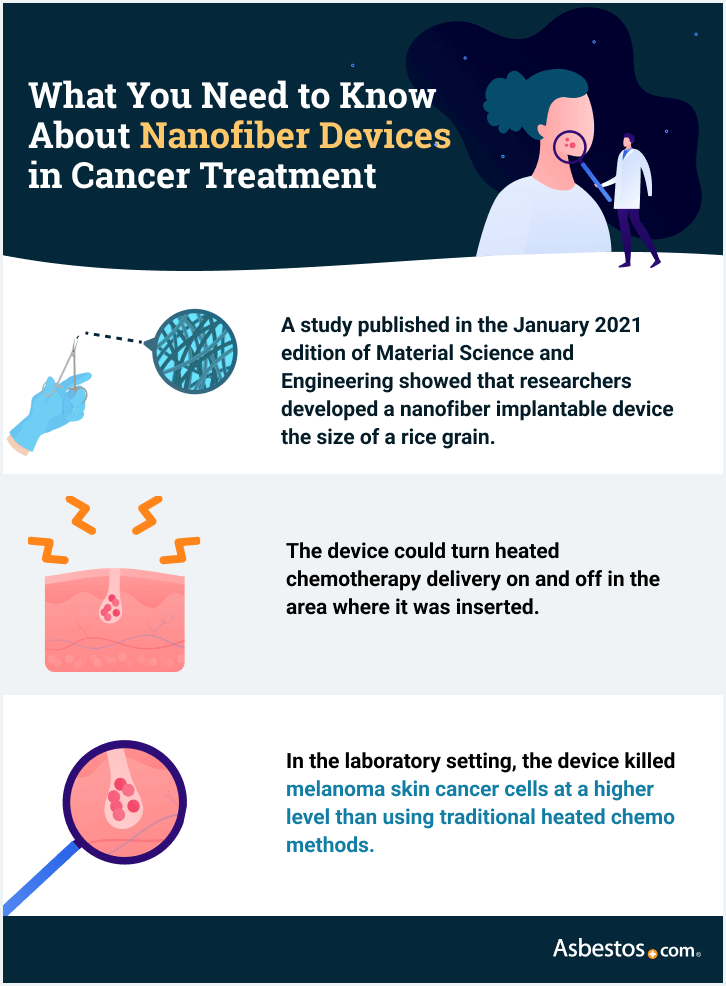
Using Nanotechnology as New Cancer Treatment
The role of nanotechnology in cancer care has focused mostly on using implantable sensors that deliver anticancer medication with greater precision than traditional methods.
Nanotechnology involves the design, production and application of incredibly small devices and systems. These devices are generally between one and 900 nanometers in length.
Visualizing how tiny that can be is nearly impossible. But for comparison, a human fingernail grows one nanometer per second. And a human hair is about 100,000 nanometers wide.
In 2022, a research team at the National Cancer Institute published their work on an innovative therapy for pleural mesothelioma using a spray-on hydrogel during surgery. The new treatment involves spraying genetically engineered nanoparticles on the cancer site to eliminate mesothelioma tumor cells left behind after surgery.
A February 2021 research study published in Emergent Materials proposed using nano-based antimicrobial technology in personal equipment to protect health care workers from viral diseases such as COVID-19.
Another team of researchers in 2020 developed a mint-sized device to regionally deliver cisplatin, a common chemotherapy drug. The lab study found the device's delivery of cisplatin was "significantly toxic" to breast and liver cancer cells.
At Memorial Sloan Kettering Cancer Center, researchers in 2019 began developing a biosensor that can be implanted in the uteruses of women at high risk of ovarian cancer.
The intrauterine device will quickly alert doctors if it detects elevated, local levels of ovarian cancer biomarkers. If development of the device is successful, it could improve early-stage diagnosis and lead to more personalized treatments.
Nanotechnology may lead the future of cancer treatment by alerting doctors of early signs of cancer, analyzing treatment effectiveness and delivering targeted therapies.
iKnife: New Cancer Fighting Technology Using Smoke
A device called an intelligent knife, also known as an iKnife, burns tissue with electricity, not a surgical blade. As the tissue burns, the iKnife collects the smoke in a tube and feeds it into an advanced computer called a mass spectrometer. That machine determines if cancer molecules are present.
A 2021 breast cancer clinical trial at Imperial College Healthcare in the UK is one of the first human trials with iKnife. A separate 2021 study in the journal Analytical Chemistry validated the iKnife's ability to differentiate tissue on par with laboratory examination.
The iKnife presents several benefits. For example, the device detects cancer molecules closer to real time instead of the days or weeks it takes for a pathologist to receive and analyze a biopsy. Doctors use tissue or cell samples taken from biopsies to learn disease information, such as cancer type.
Thanks to the near immediate analysis of cancer tissue, surgeons know whether they are cutting healthy or cancerous tissue during the surgery. This information produces a clear tumor outline in the operating room and could decrease the rate of repeat surgeries or cancer recurrence.
The iKnife can also detect the types of fat that tumors use for growth, alerting cancer patients to which fats they should avoid in their diet.
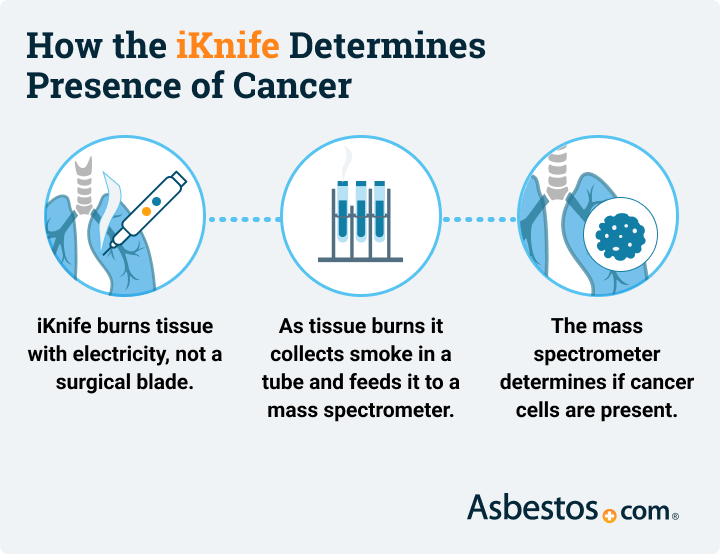
The technology in the iKnife allows doctors to remove more cancer tissue during surgery and cuts down on the need for additional biopsy procedures. Tissue analysis with the iKnife speeds up the time to meaningful treatment for patients.
Tumor Treating Fields: New Technology for Cancer Treatment
Tumor treating fields, also known as Optune or TTFields, is an evolving new cancer technology developed for treating cancer with electric fields.
TTFields are administered using a portable, lightweight device. Four adhesive patches attached to the machine are placed on the area of the body near the cancer.
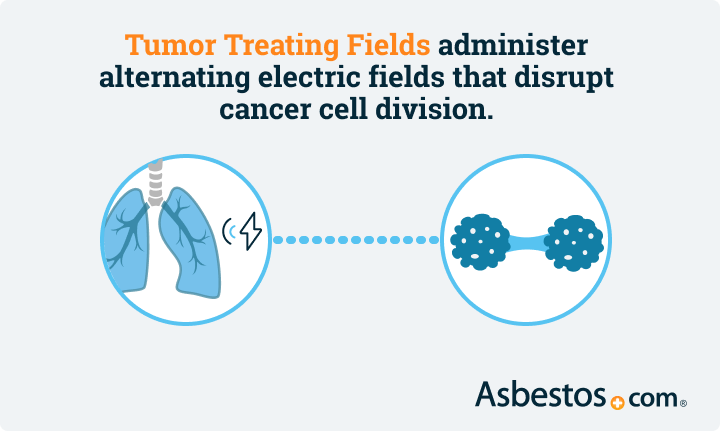
The patches then deliver low intensity, alternating electric fields to that region. The electric fields disrupt tumor cell division.
A clinical trial expected to end in 2026, dubbed TRIDENT, is studying the potential survival benefit of using tumor treating fields alongside radiation therapy and a chemotherapy drug.
TRIDENT is currently enrolling brain cancer patients at the Mayo Clinic in Arizona, H. Lee Moffitt Cancer Center and Research Institute in Tampa, Advent Health in Orlando and other cancer treatment centers in the U.S.
Tumor treating fields in 2019 received FDA approval for the treatment of mesothelioma.
The success of the latest clinical trial using tumor treating fields could shape the future of cancer treatment for patients with rare or aggressive malignancies such as glioblastoma multiforme (GBM). GBM accounts for 46% of primary brain cancers, and overall patient survival is approximately 14 months.
Tumor Treating Fields represents a new way of thinking about cancer therapy by using electrical fields with traditional medication. The technology is improving survival for brain cancer and mesothelioma patients while eliminating drug toxicity.
Source: https://www.asbestos.com/featured-stories/future-cancer-treatment/
0 Response to "Easy Information Technology Cancer Patient Senior Projects"
Post a Comment